Care begins with a detailed clinical intake, review of sleep history, and EEG brain mapping to assess brainwave activity related to sleep regulation.
Call Us: 269-430-7966
A Brain-Based Approach to Sleep Disorder Treatment
Persistent sleep problems may be rooted in how the brain regulates sleep. At Brain Treatment Center Michigan, we use EEG-guided rTMS (MeRT®) to personalize sleep disorder treatment based on your unique brain activity.

When sleep problems continue despite lifestyle changes or medication, the cause may be neurological.
Some sleep disorders are linked to how the brain regulates sleep and wake cycles. EEG-guided evaluation enables us to better understand these patterns and determine whether a brain-based approach, such as MeRT, may be appropriate.
Sleep disorders affect both adults and children and can present in a wide range of ways. Some people struggle to fall asleep, while others wake frequently throughout the night or never feel fully rested, even after adequate sleep.
Common sleep-related symptoms include:
For many people, these symptoms persist despite sleep hygiene changes, supplements, or medication.
When sleep problems continue despite lifestyle changes or medication, the cause may be neurological.

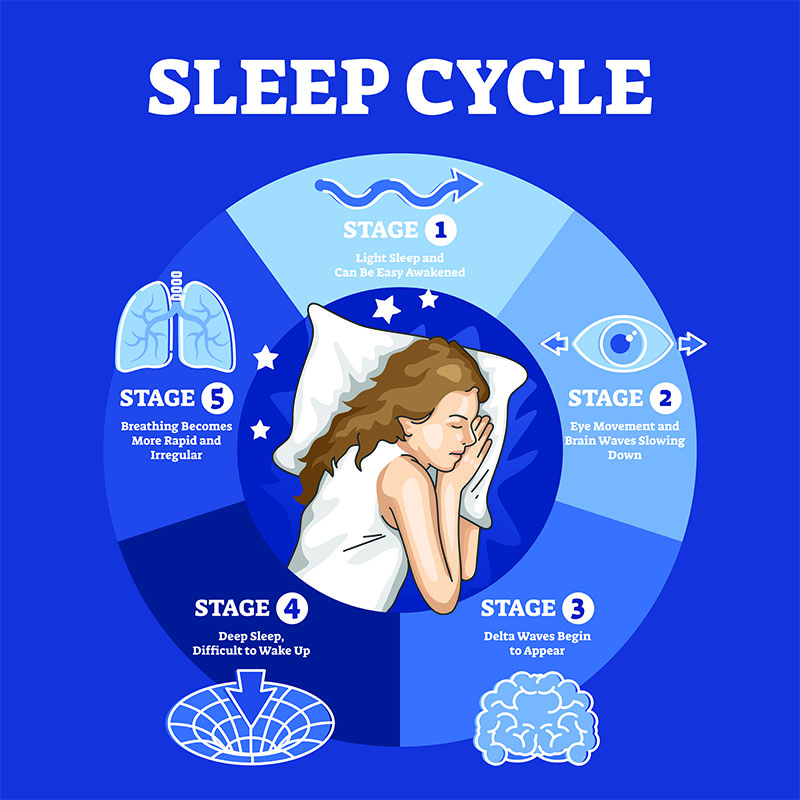
Sleep is an active neurological process regulated by complex brain networks, brainwave patterns, and natural sleep cycles.
Throughout the night, the brain cycles through lighter sleep, deeper restorative sleep, and REM sleep, each playing an important role in physical recovery, memory, and emotional regulation.
Healthy sleep requires the brain to shift smoothly between these states at the right times. When brainwave patterns are disrupted, the brain may remain in a state of hyperarousal or struggle to progress through normal sleep cycles.
This dysregulation can interfere with:
Falling asleep
Staying asleep
Reaching deeper, restorative stages of sleep
In these cases, sleep problems are often neurological rather than purely behavioral.
The Brain Treatment Centers in Marshall and Grand Rapids offer MeRT to help patients with sleep disorders.
MeRT, or Magnetic e-Resonance Therapy, is a personalized form of transcranial magnetic stimulation (rTMS) designed to address abnormal brain activity.
Traditional rTMS typically follows standardized protocols, using the same stimulation settings for many patients and targeting a limited area of the brain. While this approach can be helpful for some conditions, it does not account for individual differences in brain function.
MeRT builds on rTMS by using quantitative EEG (qEEG) brain mapping to evaluate how different areas of the brain are functioning. This information allows clinicians to identify specific patterns of dysregulation and design a treatment plan tailored to each patient’s unique brain activity.
By individualizing treatment based on objective brain data, MeRT offers a more precise and personalized approach than standard rTMS.

Traditional sleep treatments often focus on symptom management through medications, behavioral therapy, or medical devices.
Sleep disorder treatment with MeRT differs by:
MeRT is often used alongside other medical or therapeutic approaches as part of a comprehensive care plan.
MeRT has shown some incredible results in treating sleep disorders
To find out if MeRT is the right choice for you, reach out to our New Patient Coordinator. She can provide detailed information about the treatment, protocols, costs, and payment options. If you decide to proceed, here’s what comes next…
Care begins with a detailed clinical intake, review of sleep history, and EEG brain mapping to assess brainwave activity related to sleep regulation.
We use your EEG data to develop an individualized MeRT protocol based on your specific brain patterns.
Your rTMS sessions are outpatient, non-invasive, and do not require anesthesia or medication. Sessions are typically brief and completed over several weeks.
Your clinician monitors your progress throughout treatment, and we take follow-up EEGs to evaluate changes and adjust treatment as needed.

Chronic sleep problems can be difficult to navigate, especially when they persist despite lifestyle changes or traditional treatments.
Understanding whether disrupted brain activity may be contributing to sleep issues is an important step.
Our New Patient Coordinator can
"*" indicates required fields